Local cardiac arrest data informed Lynn Blake’s strategy to determine AED locations that contributed to a timely save
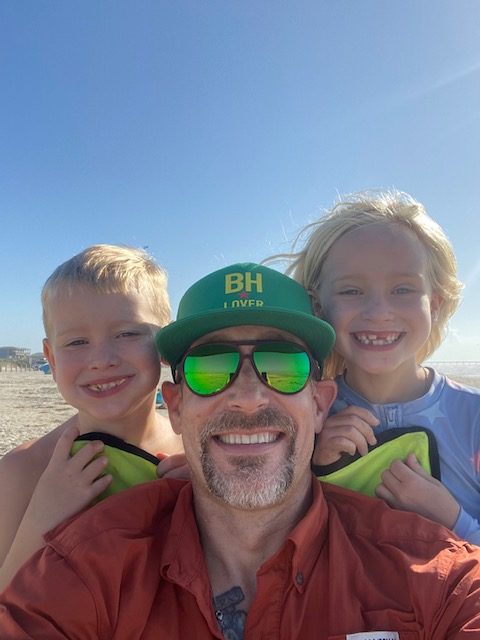
Last July, Doug Schwartz was enjoying dinner with his girlfriend, Shelly Belknap, and a friend at eTown restaurant located in Edwards, Colorado when he began to feel faint, and he suddenly suffered a cardiac arrest.
Shelly, who is an oncology nurse at Vail Health, was sitting next to Doug and immediately started CPR. Stephen McGaffick, an employee at eTown who is also a Beaver Creek Ski Patrol member, took turns with Shelly and performed CPR on Doug.
Fortunately, an automated external defibrillator (AED) was located about 100 yards away outside in a heated box attached to a lamppost in the Riverwalk, which is Edwards’ downtown area.

A restaurant patron named Megan went to go grab the AED. When Megan returned with the AED, Shelly and Steve applied the device, which delivered two shocks by the time the paramedics arrived.
The paramedics took over and helped revive Doug. The restaurant patrons, who anxiously waited for an update on Doug’s condition, erupted into applause once they heard that he was alert.
Doug was transported by ambulance to Vail Health Hospital and then transported by helicopter ambulance to Denver that night. He spent five days in the ICU at Medical Center of Aurora and was then discharged.
Placing AEDs in key locations can make the difference between life and death. A person’s chance of survival decreases by 7 to 10 percent for every minute that passes without defibrillation.
The AED used to help save Doug’s life was one of more than 100 devices that had been strategically placed throughout Eagle County, Colorado about seven years ago thanks to the efforts of a local resident named Lynn Blake, a strong advocate for public AED implementation programs and quality improvement initiatives for cardiac arrest outcomes.
“I was flooded with emotions for a man I never met,” Lynn said when she learned that Doug’s life had been saved thanks to CPR and the use of the AED. “He was the reason I devoted so much of my life to implementing these programs, it was all for this man and his family.”
Lynn’s journey with advocating for the AED program in Eagle County traces back to her own personal story as a cardiac arrest survivor.
Surviving a Cardiac Arrest Spurs CPR and AED Advocacy Work
The start of 2007 was a whirlwind for Lynn. She got married on Feb. 3 and went on her honeymoon two days later. As soon as she returned from her trip, she began a new job in Vail, which is also located in Eagle County.
On Feb. 14, 2007, Lynn, 27, was on the second day of her job when she suddenly experienced cardiac arrest. One of Lynn’s co-workers, Sue Froeschle, whom Lynn hadn’t even met yet, immediately started CPR while another employee called 911 and ran to get help from the Vail Fire station that was across the street. Eagle County paramedics were also nearby; they quickly arrived and used a defibrillator to deliver three shocks to her heart.

Lynn survived the incident and now has an implantable pacemaker defibrillator. She finally met Sue a year later when the American Heart Association gave an award to the first responders who helped save Lynn’s life. After the event, Lynn and Sue became very close. Her son is even named Thomas Froeschle Blake.
“There were so many coincidences and ironic details that allowed me to survive – I felt so compelled and convinced that my life was saved for a reason,” Lynn said.
Lynn didn’t know anything about cardiac arrest before the incident. She started researching to learn more about the condition. She also became an American Heart Association CPR instructor so that she could teach others how to save lives.
Throughout those early days of investigating, Lynn learned that cardiac arrest is a leading cause of death in the U.S. Yet, she was confounded that she couldn’t find any data on incidences and outcomes anywhere.
“No one could tell me who experiences cardiac arrest in Eagle County or even Colorado,” she recalled. “I could not find any information that was truly validated. Everything was an estimate.”
It wasn’t until she read a book titled, “Resuscitate,” that she learned about the Cardiac Arrest Registry to Enhance Survival (CARES), a quality improvement program that works with EMS communities to collect data and measure out-of-hospital cardiac arrest outcomes.
After connecting with CARES and learning more about the program, she worked with local health authorities and volunteers to secure funding so that Eagle County could participate in the registry starting in 2014. She then worked with officials to get the state of Colorado to participate in CARES in 2019.
Lynn said it’s imperative to track how bystanders and EMS are responding to cardiac arrest to identify the necessary intervention strategies that will optimize the chain of survival.
“I can’t say ‘you need to learn CPR and have an AED’ if we don’t know if people are performing CPR and using AEDs,” she said. “It’s impossible to improve resuscitation outcomes if you don’t know what you’re improving. Data collection allows not only the community to figure out how citizens should be engaged, but also gives agencies a way to measure their performance. Quantitative analysis of cardiac arrest is the linchpin to successful resuscitation, and it must happen for the conversation to continue.”
Using Data to Guide AED Placement in Eagle County
Out-of-hospital cardiac arrest (OHCA) is a global public health issue experienced by 3.8 million people annually. Only 8% to 12% survive to hospital discharge. Early defibrillation of shockable rhythms is associated with improved survival, but ensuring timely access to defibrillators has been a significant challenge.
Public-access defibrillation is the use of AEDs by the public to facilitate CPR and early defibrillation before professional responders arrive. A recent International Liaison Committee on Resuscitation (ILCOR) scientific statement commissioned by the American Heart Association evaluated the barriers to public-access defibrillator use and early defibrillation. The statement titled, “Optimizing Outcomes After Out-of-Hospital Cardiac Arrest With Innovative Approaches to Public-Access Defibrillation,”also identified the opportunities for new approaches to public-access AED program implementation.
Public-access defibrillation has saved many lives. Unfortunately, public-access AEDs still remain underused. The devices are used in less than 3% of OHCAs.
However, people who experience OHCA with a nearby AED are three times more likely to receive bystander defibrillation and twice as likely to survive as those without an AED nearby, according to the statement. Unfortunately, AEDs are rarely close enough for timely retrieval. The issue is further compounded by the fact that even when a registered AED is near a cardiac arrest incident, most go unrecognized and unused. The ILCOR statement calls for using innovative approaches to improve public-access defibrillation in the future by optimizing AED availability, reliability and usability through coordinated, data-driven, regional strategies.
When Lynn worked with officials in various Eagle County communities to place the more than 100 AEDs, it was important to them that the devices were easily accessible and not placed behind locked doors like they had typically been in the past.
However, she said there was some initial reluctance among entities to place public defibrillators, especially outside and unsecured. She said the entities feared liability, theft, people using them unnecessarily, and freezing temperatures.
Through education efforts, Lynn helped the entities understand the crucial need for AEDs by sharing statistics and the fact that theft is fairly uncommon. She worked to ensure that the AEDs were placed outside in heated boxes attached to lamp posts where they’d be available 24/7.
Additionally, the ILCOR statement discusses the value of geographic cardiac arrest data to inform AED placements such as density maps of OHCAs that plot incidences on a map that can pinpoint higher-risk spots for cardiac arrest and prime locations for AEDs.
Using data from CARES, Lynn said AEDs were placed in the most common public locations for cardiac arrest emergencies such as healthcare/nursing home facilities, schools and libraries throughout the county. Then, the most highly-trafficked public places were identified using Eagle County’s geographic information system and Google maps. Lynn said it wasn’t realistic to place a unit in every small business, plus the lifesaving devices needed to be accessible 24/7.
“This started the outdoor cluster approach, installing heated cabinets to light posts in the most centrally accessible points to multiple establishments,” she said. “Deploying one unit for numerous places significantly diminishes the cost and increases accessibility. “
Lynn said she worked with her neighborhood of EagleVail to install defibrillators at major residential and golf/Nordic course intersections because CARES data suggests that residences are the most commonplace for cardiac arrests to occur.
“Hopefully, someday in the near future, defibrillators will be as common as microwaves in homes,” she said. “Until then, we must continually strive for the ubiquity of these lifesaving devices. There is so much more that can be done, but working from the grassroots up is very difficult. Federal mandates and more awareness must occur to achieve the availability needed.”
‘It Took a Village to Save Doug’

In December, Lynn and Doug met for the first time at a coffee shop.
“I was very grateful,” Doug said. “That is what I tried to communicate to Lynn in my meeting. It is strange to sit across the table from somebody who played a part in saving your life.”
He said he feels very fortunate with the way the events unfolded last July from receiving high-quality, immediate CPR from Shelly to Megan grabbing the AED nearby.
“I don’t know how you could draw up a plan any better with the timeliness of my save,” he said.
For Lynn, it was a dream come true to meet Doug whose life was saved with the help of an AED program that she and other volunteers developed after she received a second chance at life. It’s also a testament to the chain of survival that improved once the community started tracking and measuring data to make changes that save lives.
“It took a village to save Doug,” she said. “There are so many components that have to take place to save one life.”